Vertebral instability
The definition of vertebral instability is the impossibility for the vertebral column to protect the medulla and the nerves when it is under physiological load. Numerous pathologies could provoke a vertebral instability, for example, a vertebral fracture, a tumor, or a degenerative disease.
The evaluation of stability or instability is based on precise criteria after acquisition of CT scan and MRI. A dynamic radiography could also be necessary. Depending on this clinical and radiological assessment, the neurosurgeon could quantify the grade of instability of the column.

Trans-muscular approach for decompression
In case of minor instability, a conservative treatment could be enough, which is a bed rest or the wearing of an orthosis depending on the localization of the instability. This treatment is for a period of 6-12 weeks and necessitates a regular radiological follow-up.
In case of major instability, a surgery of stabilization is necessary. The most common technique is the trans-peduncular screw placement with the goal to make a bridge between the vertebrae above and below the pathologic one. With this treatment, the patient do not need any orthosis. Dr Robert and Dr Bonasia realize this surgery under microscopic view and with a minimal invasive technique to limit the muscular trauma. Their surgical experience for lumbar herniated disk is more than 600 cases.
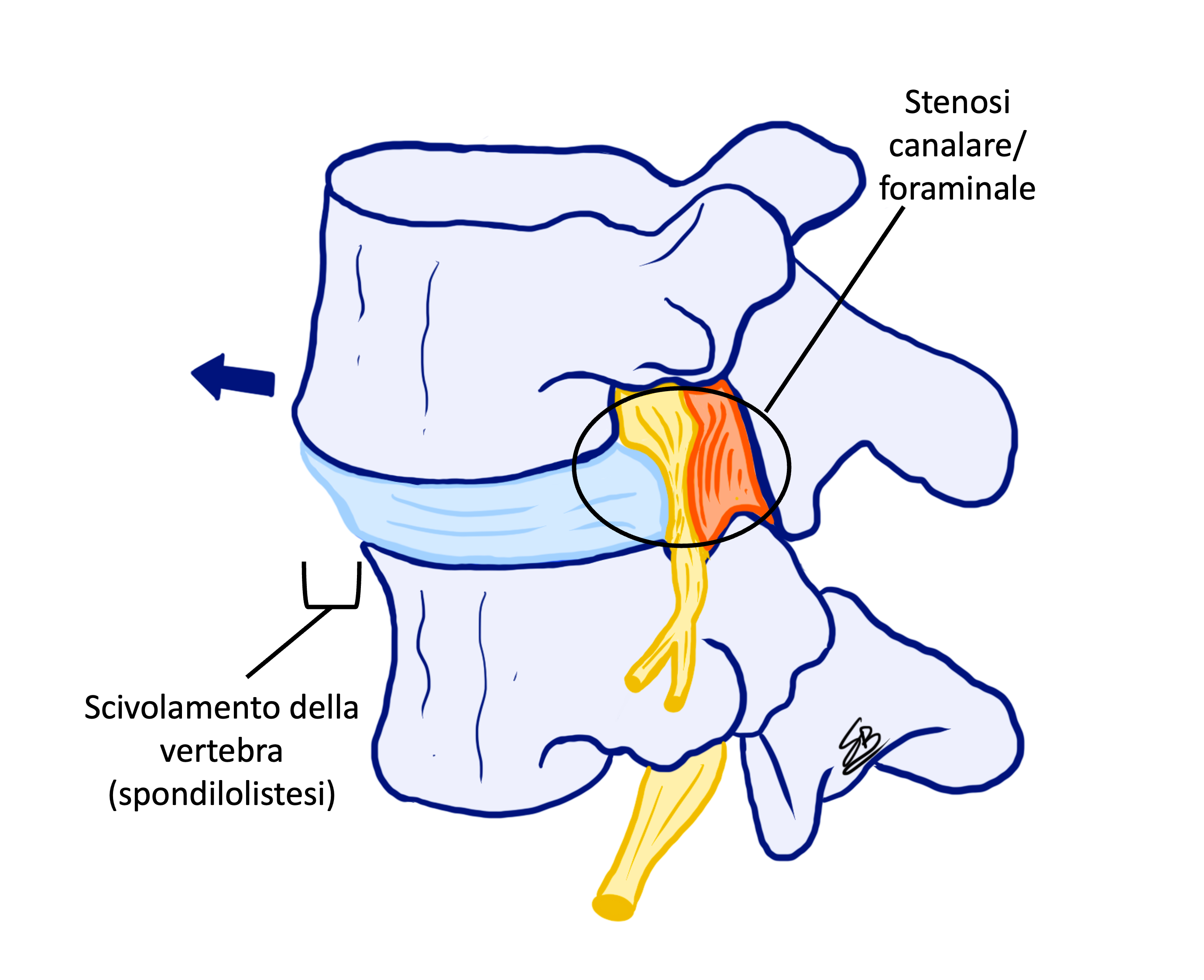
Vertebral segment after stabilization TLIF
After a surgery of vertebral stabilization, the patient follows one cycle of physiotherapy, and the convalescent period is 1 month long. We propose a follow-up of 1 year after such treatment.